|
Revista Ciencias de la Actividad Física UCM, 23(1), enero-junio, 2022.
ISSN: 0719-4013
Exercise may improve balance on
Parkinson patients El ejercicio puede mejorar el equilibrio en los pacientes de Parkinson
1 Bruna Alexandra de Souza de Oliveira, 2 Walmir Romário dos Santos,
3 Isac Alexandre Ferreira da Silva, & 4 Wlaldemir Roberto dos Santos
De Souza, B. A., dos Santos, W. R., Ferreira-Silva, I. A., & dos
Santos, W R. (2022). Exercise may improve balance on Parkinson
patients. Revista Ciencias de la Actividad Física UCM, 23(1),
enero-junio, 1-7. https://doi.org/10.29035/rcaf.23.1.1
RESUMEN La enfermedad de Parkinson deteriora la capacidad funcional del paciente al afectar su coordinación motora y el equilibrio, lo que puede provocar caídas y, en consecuencia, morbilidades asociadas o incluso la muerte. De esta manera, las terapias auxiliares de la terapia farmacológica, como los programas de ejercicio físico que buscan mejorar la coordinación y el equilibrio, pueden ayudar a evitar el riesgo de caídas y, por lo tanto, mejorar la calidad de vida de las personas afectadas por esta enfermedad. Por tanto, el presente estudio tiene como objetivo verificar la efectividad de un programa de ejercicios de cuatro semanas que incluye ejercicios de equilibrio y coordinación motora para mejorar el equilibrio de las personas con Parkinson, utilizando la escala de Berg. Doce personas (64,18 ± 9,54 años; 73,83 ± 14,97 kg; 168,25 ± 8,24 cm) se sometieron a dos sesiones semanales de ejercicios divididos en tres series de 90 segundos para cada ejercicio, para un total de ocho sesiones. La puntuación de los individuos en la escala de Berg aumentó significativamente (p = 0,033) de 43,58 ± 6,53 a 46 ± 5,22. Sabiendo que los puntajes inferiores a 45 significan una probabilidad considerable de caídas, es posible afirmar que el programa de ejercicio aplicado fue efectivo para mejorar el equilibrio de los individuos y, en consecuencia, puede conducir a una mejora en la capacidad funcional del individuo y una posible mejora en la calidad de vida. Palabras clave: Parkinson, Equilibrio, Ejercicio físico. ABSTRACT Parkinson’s disease can harm the functional capacity of a person, which may lead to a worse motor coordination and balance, increasing the risk of falls, and consequently to morbidities or even death. So, complimentary therapies to the drug therapy as exercise programs the aim to increase coordination and balance may avoid the possible falls that may occur and to increase the life quality for people with this illness. Thus, the present study is aimed to verify the efficiency of a four-week exercise program formed by balance and motor coordination on people living with Parkinson using Berg scale to evaluate it. Twelve individuals (64.18 ± 9.54 years; 73.83 ± 14.97 kg; 168.25 ± 8.24 cm) were submitted to two sessions each week consisted of exercises divided in three series of 90 seconds, in a total of eight sessions. The Berg scores increase significatively (p = 0.033) from 43.58 ± 6.53 to 46 ± 5.22. Since scores less than 45 mean a high probability of falls, it is possible to say that the applied program was effective in increase the balance for these individuals, consequently, leading to a better functional capacity and a possible better life quality. Key words: Parkinson's, Balance, Physical Exercise. 1 Graduation in Physical Education. Centro Universitário FBV Wyden, Recife – PE / Brasil https://orcid.org/0000-0002-7397-010X | brunaalexandra_@hotmail.com 2 Master in Physical Education. Universidade de São Paulo, Ribeirão Preto – SP / Brasil https://orcid.org/0000-0001-5558-3109 | walmir@wrsantos.br 3 PhD in Physiology. Secretaria de Educação do Estado de São Paulo, Ribeirão Preto – SP / Brasil. https://orcid.org/0000-0001-5222-1444 | isacferreira@prof.educacao.sp.gov.br 4 PhD in Sciences. Universidade Estadual da Paraíba, Campina Grande – PB / Brasil https://orcid.org/0000-0001-5706-2243 | wlaldemir@hotmail.com INTRODUCTION The Organização Mundial da Saúde (2015), estimates a significant increase in world life expectancy. However, the increased longevity raises the probability of chronical diseases. Parkinson’s Disease has been one of the most frequently reported among the elderly and, in Brazil, almost 200 thousand individuals living with this condition (Associação Brasileira de Neurologia, 2020). Parkinson’s disease is a progressive degenerative disease caused by the diminished dopamine production, impacting on the voluntary movements, mostly in aging people (Associação Brasil Parkinson, 2020). It features shaking, movement reduction, lack of balance and stiffness, leading to problems in walking, functional incapacity and, as consequence, decreased autonomy and life quality (Dias & Limongi, 2003). Cunha & Lourenço (2014) state the changes by Parkinson´s disease increase the risk of falling, that may lead to an increase in morbidity and mortality rates. Nowadays, drug treatment is the disease’s standard treatment, however, it has been noted a decreased efficiency of this practice in time, which may be related to the development of motor problems associated to this illness (Fabbrini et al., 2007). Thus, it is needed to implement combined therapies such as physical exercises, which contributes to movement control and reduce the disease’s progression (Crizzle & Newhouse, 2006; Robichaud & Corcos, 2005). According to the Portuguese Association of Parkinson's Patients (Parkinson APdDd, 2016) exercise programs to Parkinson’s disease patients must include stretching, balance, motor coordination and strength exercises. Thus, the exercise program may positively aid in the illness control, helping to an increase functional capacity, balance and walking, reducing the risk of falling, leading to better self-esteem and life quality (Oxtoby, 2016). Since a significant amount of elderly population have Parkinson’s disease and it may decrease functional capacity, increasing the number of falls and its complications, leading to morbidity and mortality, and physical exercise is described as fundamental to treat this condition, this study aimed to verify the effectiveness of functional exercises, motor coordination and balance program in people with this disease. METHODS Subjects and Study Design The sample consisted of 12 individuals characterized as in Table 1. They were invited to voluntarily participate in this study and were informed of all risks and benefits. All of the included signed the informed consent that they were inserted in the multi professional follow up at Associação de Parkinson de Pernambuco (ASP-PE), they did not have any illness that could comprise cardiovascular responses and/or joint range limitations which could preclude their participation in physical exercises. The procedures followed the ethical rules stated in resolution 466/12 and were approved by the Ethics and Research Committee of the University Center of Vale do Ipojuca (CAE: 62532716000005666). After subject selection, they were submitted to Berg’s balance test to evaluate fall risk. Then, a four-week training protocol were applied and, when finished, Berg’s balance test was reapplied. Sample Characterization Age, height, body mass, Parkinson’s diagnosis time, Parkinson’s treatment and acitivity level (considering physically active those who performed at least 150 minutes of moderate or vigorous intensity weekly; Organização Mundial da Saúde, 2020) were evaluate from previous questionnaire on ASP-PE. The data is summarized on Table 1. The original sample consisted of 27 elderly included in ASP-PE. They were classified using Hoehn and Yahr Scale (Degree of Disability Scale) in five stages of the disease and only people on stages 3 (light to moderate bilateral disease; some postural instability or independent living) and 4 (server incapacity, but still capable of walking and standing without help). The final sample consisted in 12 subjects, all of them underwent to the exercise program accompanied by a physical educator and authorized by a physician. Training Protocol The four-week training protocol was conducted in two weekly sessions (Tuesdays and Thursdays) of 60 minutes, making up a total of eight sessions at the end the study. It was divided in 1) warmup: dynamic and static stretching; 2) main session: balance exercises as proposed by (Dawes & Roozen, 2011), following this order: walk in line, steps forward and backwards over the line, lateral steps over the line, lateral steps forward and backwards over the line, two feet on each space of a ladder, sit and up in a chair. All exercises were performed in three series lasting 90 seconds each with 60 seconds intervals between series, and; 3) cool-down using static stretching. Berg’s Balance Test Berg’s balance test was developed by Katherine Berg in 1992 and adapted to Portuguese speaking countries by Miyamoto et al. (2004). The aim is to evaluate balance and, along that, estimate the risk of falling. The test is made of 14 items, each one with five possible answers that correspond to scores from zero to four points, being zero the inability of completing the mentioned task and four the complete ability of doing that. The maximum score is 56 points and a score below 45 indicates a possible fall and below or equal to 36 points is associated to a 100% of fall risk (Miyamoto et al., 2004; Hayes & Johnson, 2003). Statistical Analysis The sample was characterized by a descriptive analysis expressed by mean values and standard deviation. For intragroup comparison (before and after training) the Paired T test was used. All analysis was conducted using Statistical Package for the Social Sciences - SPSS 17.0 software, with significant level set at p<0.05. RESULTS Twelve subjects were evaluated, six of each sex, they were submitted to eight exercise sessions, lasting one hour, twice a week. The data from the subjects are described on Table 1. Table 1 Sample Characterization. 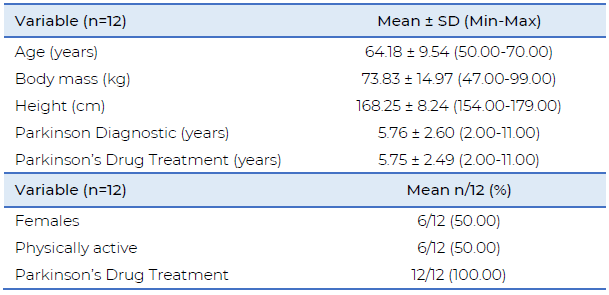 When before and after exercise values are compared, it is observed a significant increase in Berg’s balance scale by 5.55% (p=0.033; Table 2). Table 2 Berg’s scale of balance before and after the training protocol. 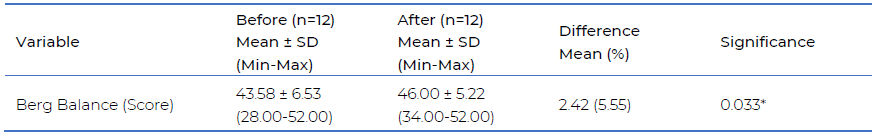
*p<0,05
Looking at the individual data, just two subjects did not have positive changes after the training protocol, being 17% of the sample (Table 3). Table 3 Individual values from Berg Scale for each of the 12 participants (pre e post-test). 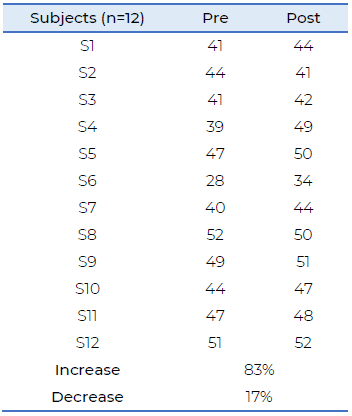 DISCUSSION The present study verified the impact of a functional exercise program, involving motor coordination and balance in individuals with Parkinson's disease. The results indicate a better balance after the proposed protocol (p=0.033), thus, there was a decrease in the risk of falling. Before the training protocol the subjects had a mean score of 43.58 ± 6.53 in Berg’s scale of balance, where scores below 45 indicate increased risk of falling (Silva et al., 2008; Miyamoto et al., 2004; Hayes & Johnson, 2003). After the exercise, the mean score increased to 46 ± 5.22, showing a lower risk of falls. According to the Organização Mundial da Saúde (2015), regular exercise for elderly population is a powerful tool to improve several aspects of health, including improves in balance. To achieve that, regular and organized training are needed to improve the performance on this population. The initial hypothesis is that elderly people with Parkinson display a higher fall rate than healthy elderly people, as the literature states. In a study with 39 elderly patients with Parkinson (stages 2 and 3), Ribeiro & Pereira (2005) applied a strength training with instability for 12 weeks and, using Berg Balance Scale, found improvement on mobility, cognition, balance, marching, with no changes in the number of falls in this specific group. In the same direction, Reuter et al. (1999) followed a group of eight patients for eight months, applying a physical training protocol aiming the improvement of motor coordination and balance, not finding any improvement with the intervention, through basic motor test (test for muscle strength, flexibility, and coordination). However, the exercises maintained the clinical condition of all participants. According to the findings from this study, Oxtoby (2016) point that physical exercise is an important aid on Parkinson’s control, helping to a better balance and walking, reducing the risk of falling. So, it is important to develop therapeutics programs to reduce the risk of falls in this population, since the falls may cause fractures, increase in dependence, morbidity, and mortality (Cunha & Lourenço, 2014). Ribeiro & Pereira (2005) found a decreased risk of falling in elderly people by Berg Balance Scale (p=0.05), after 27 sessions of balance training. As in this study, Chaves et al. (2011) in a longer training period, 20 weeks, found that Parkinson’s patients increased balance and reduced the risk of falls (p=0.001), using Berg Balance Scale. Lun et al. (2005), submitted 19 women with Parkinson to an eight-week supervised exercise program and, after that, they improved their motor coordination and balance, identified by Berg Balance Scale and Timed Up and Go Test. Chaves et al. (2011) evaluate the functional performance of ten Parkinson’s patients that were submitted to functional training, three times a week, and after the proposed training, an increased functional condition was displayed (p=0.003), identified by the modified functional performance test. Using a global exercise plan for a 16-month period, Schenkman et al. (2012), found that all patients performed better in daily tasks involving balance, observed in Functional Reach Test. It is clear in the literature that a better balance in Parkinson’s patients lead to a better functional condition, which improve the overall motor condition and decreases the risks of falling and associated comorbities (Oxtoby, 2016; Cunha & Lourenço, 2014). The strengths observed in the present study: using a standardized classification for the sample with a systematized and extended intervention plan, however, studies with larger samples are suggested to better show such results, this is a limitation of our research. CONCLUSIONS Parkinson’s disease highly affects the functional capacity from people, decreasing their autonomy and life quality. This balance improvement, caused by the disease, increases the risk of falling, and consequently increasing morbidities and mortality rates. This study demonstrates that functional exercises involving strength and motor coordination are a good way to improve balance in Parkinson's patients, reducing the risk of falls. Because of that, it is proposed that an exercise program focused and designed for Parkinson’s patients may increase their quality of life and reduce the risks of morbidities and casualties due to the falls caused by the illness progression. However, it is suggested that more studies should be conducted about the benefits of exercise programs in this specific population. REFERENCES Associação Brasil Parkinson. (2020). O que é Parkinson?. http://www.parkinson.org.br Associação Brasileira de Neurologia. (2020). Conheça os sintomas do mal de Parkinson. http://abneuro.org.br Chaves, C. M. C. M., Mitre, N. C. D., & Liberato, F. A. (2011). Efeitos de um Programa de Fisioterapia em Pacientes com Doença de Parkinson. Revista Neurociências, 19(3), 484-90. https://doi.org/10.34024/rnc.2011.v19.8358 Crizzle, A. M., & Newhouse, I. J. (2006). Is physical exercise beneficial for persons with Parkinson's disease? Clinical Journal of Sport Medicine, 16(5), 422-5. https://doi.org/10.1097/01.jsm.0000244612.55550.7d Cunha, A. A., & Lourenço, R. A. (2014). Quedas em idosos: prevalência e fatores associados. Revista Hospital Universitário Pedro Ernesto, 13(2), 21-9. https://doi.org/10.12957/rhupe.2014.10128 Dawes, J., & Roozen, M. (2011). Desenvolvendo velocidade e agilidade (1a Ed.). Manole. Dias, A. E., & Limongi, J. C. P. (2003). Tratamento dos distúrbios da voz na doença de Parkinson: o método Lee Silverman. Arquivos de Neuro-Psiquiatria, 61(1), 61-6. https://doi.org/10.1590/S0004-282X2003000100011 Fabbrini, G., Brotchie, J. M., Grandas, F., Nomoto, M., & Goetz, C. G. (2007). Levodopa‐induced dyskinesias. Movement disorders, 22(10), 1379-89. https://doi.org/10.1002/mds.21475 Hayes, K. W., & Johnson, M. E. (2003). Berg balance scale. American College of Rheumatology, 4(1), 28-30. https://doi.org/10.1002/art.11411 Lun, V., Pullan, N., Labelle, N., Adams, C., & Suchowersky, O. (2005). Comparison of the effects of a self‐supervised home exercise program with a physiotherapist‐supervised exercise program on the motor symptoms of Parkinson's disease. Movement disorders: official journal of the Movement Disorder Society, 20(8), 971-5. https://doi.org/10.1177/0269215509358933 Miyamoto, S. T., Lombardi Júnior, I., Berg, K.O., Ramos, L.R., & Natour, J. (2004). Brazilian version of the Berg balance scale. Brazilian Journal of Medical and Biological Research, 37(9), 1411-21. https://doi.org/10.1590/S0100-879X2004000900017 Oxtoby, M. (2016). Tudo sobre doença de Parkinson: respostas às suas dúvidas (1. Ed.). Editora Andrei. Parkinson APdDd (2016). Programa de exercícios. http://www.parkinson.pt Reuter, I., Engelhardt, M., Stecker, K., & Baas, H. (1999). Therapeutic value of exercise training in Parkinson’s disease. Medicine & Science in Sports & Exercise, 31(11), 1544-9. https://journals.lww.com/acsmmsse/Fulltext/1999/11000/Therapeutic_value_of_exercise_training_in.8.aspx Ribeiro, A. S. B., & Pereira, J. S. (2005). Melhora do equilíbrio e redução da possibilidade de queda em idosas após os exercícios de Cawthorne e Cooksey. Revista Brasileira de Otorrinolaringologia, 71(1), 38-46. https://doi.org/10.1590/S0034-72992005000100008 Robichaud, J. A., & Corcos, D. M. (2005). Motor deficits, exercise, and Parkinson's disease. Quest, 57(1), 79-101. https://doi.org/10.1080/00336297.2005.10491844 Schenkman, M., Hall, D. A., Barón, A. E., Schwartz, R. S., Mettler, P., & Kohrt, W. M. (2012). Exercise for people in early-or mid-stage Parkinson disease: a 16-month randomized controlled trial. Physical Therapy, 92(11), 1395-410. https://doi.org/10.2522/ptj.20110472 Silva, A. D., Almeida, G. J., Cassilhas, R. C., Cohen, M., Peccin, M. S., Tufik, S., & Mello, M. T. (2008). Equilíbrio, coordenação e agilidade de idosos submetidos à prática de exercícios físicos resistidos. Revista Brasileira de Medicina do Esporte, 14(2), 88-93. https://doi.org/10.1590/S1517-86922008000200001 Organização Mundial da Saúde. (2015). Resumo. Relatório mundial de envelhecimento e saúde. https://apps.who.int/iris/bitstream/handle/10665/186468/WHO_FWC_ALC_15.01_por.pdf?sequence=6 Organização Mundial da Saúde. (2020). World Health Organization. Physical activity. https://www.who.int/news-room/fact-sheets/detail/physical-activity Dirección para correspondencia
Bruna Alexandra de Souza de Oliveira
Graduation in Physical Education Centro Universitário FBV Wyden Recife – PE / Brasil ORCID: https://orcid.org/0000-0002-7397-010X Contacto: brunaalexandra_@hotmail.com Recibido: 18-02-2021 Aceptado: 01-03-2021
|
